For new mothers, ensuring their infant receives adequate nourishment is a paramount concern. However, anxieties surrounding overfeeding can cloud this initial period. This article delves beyond simplistic stereotypes, exploring the physiological and behavioral signs that may indicate an infant is receiving excessive nourishment. We will also discuss strategies for fostering responsive feeding practices that promote healthy development.
The Detriments of Overfeeding
While occasional instances of overfeeding are unlikely to cause lasting harm, consistent practices can lead to a cascade of discomforts and potential health complications for the infant, including:
- Gastrointestinal Distress: An overloaded digestive system struggles to cope, manifesting as spitting up, gas, bloating, and diarrhea.
- Fussiness and Crying: A full stomach can be as unpleasant as an empty one for an infant, triggering prolonged crying episodes and increased fussiness.
- Sleep Disruption: Discomfort from overfeeding can significantly disrupt sleep patterns, leading to shorter naps and difficulty settling for nighttime sleep. This lack of quality sleep can further exacerbate daytime crankiness.
- Weight Gain Issues: Over time, consistent overfeeding can contribute to the development of childhood obesity, which carries a multitude of health risks later in life.

Moving Beyond Stereotypes
It’s important to move beyond the stereotype that equates a “good mother” with a constantly full baby. Most infants possess an inherent ability to regulate their intake. By observing their cues and fostering responsive feeding practices, mothers can nurture the development of healthy eating habits from the very beginning.
Decoding Infant Communication
Each infant is unique and will exhibit individual feeding patterns. However, some common indicators suggest a baby might be consuming more than necessary:
- Frequent Spit-Up or Projectile Vomiting: While some degree of spitting up is normal for newborns (due to an immature digestive system), excessive amounts or forceful vomiting episodes warrant evaluation for overfeeding.
- Persistent Fussiness After Feeding: If an infant cries consistently following a feeding session, it might signal discomfort from a full stomach rather than hunger pangs. Observing their body language for signs of distress, such as clenched fists or arched backs, can provide additional clues.
- Excessive Burping: Frequent burping, even after proper burping techniques have been employed, can be a sign of overfeeding. This suggests air intake due to rushed feeding or offering too much milk at once.
- Difficulty Settling for Sleep: Discomfort from a full stomach can make it challenging for an infant to fall asleep or stay asleep for extended periods. This can lead to a vicious cycle of fatigue and frustration for both mother and baby.
- Rapid Weight Gain: While healthy weight gain is expected in infants, excessive or rapid gain can be a potential indicator of overfeeding. Pediatricians track weight gain on growth charts to ensure it falls within the appropriate percentiles.
Fostering Responsive Feeding Practices
By implementing responsive feeding techniques, mothers can nurture a healthy relationship with food for their babies:
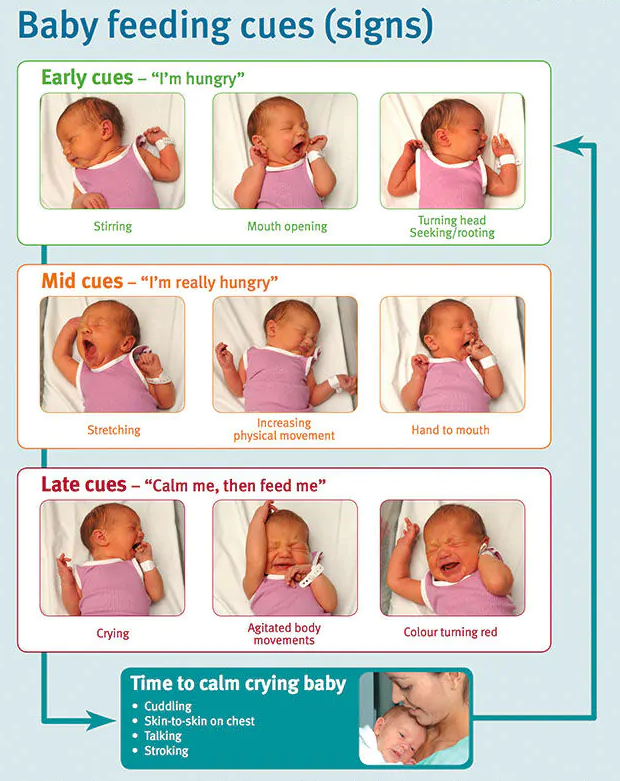
- Decoding Hunger Cues: Learning to recognize early hunger cues like rooting, sucking motions, and hand-to-mouth movements is essential. Feeding based on these cues, rather than a rigid schedule, allows for a more natural feeding pattern and reduces the risk of overfeeding.
- Observing Satiety Cues: Once feeding commences, it is crucial to pay close attention to satiety cues. These may include turning away from the breast or bottle, closing fists, or slowing down suckling. Respecting these cues allows the baby to regulate their intake and fosters a sense of control.
- Utilizing Pacifiers for Comfort Sucking: Sometimes, an infant’s cries stem from a need for comfort sucking rather than hunger. Offering a pacifier can satisfy this reflex without introducing additional milk intake.
- Avoiding Pressure to Finish: There is no need to force an infant to finish a bottle or completely empty the breast. Allowing them to determine their own feeding volume fosters a sense of control and reduces the risk of overfeeding.
- Trusting Maternal Intuition: As mothers bond with their infants, a strong intuition regarding their needs develops. If a mother feels their baby might be overfed, consulting with a pediatrician is always advisable. Open communication with the pediatrician allows for personalized guidance and reassurance.
Collaboration is Key
When concerns regarding feeding practices or weight gain arise, consulting with a pediatrician is the most prudent course of action. Pediatricians can assess the infant’s growth and development, provide personalized guidance tailored to the specific situation, and address any underlying medical conditions that might be contributing to feeding difficulties. Additionally, lactation consultants can offer valuable support and strategies for breastfeeding mothers.
Addressing Underlying Issues
Beyond simply identifying overfeeding, it’s crucial to explore potential underlying issues that might be contributing to feeding difficulties. Here are some considerations:
- Tongue Tie or Oral Ankylosis: This condition restricts the tongue’s movement due to a shortened frenulum, the tissue tethering the tongue to the floor of the mouth. In some cases, tongue-tie can interfere with effective breastfeeding, leading to frustration and potentially causing the mother to overfeed in an attempt to compensate. A simple frenotomy procedure can address this issue.
- Gastroesophageal Reflux Disease (GERD): GERD is a condition where stomach contents reflux back into the esophagus, causing discomfort. This discomfort can be misinterpreted as hunger, leading to overfeeding. Pediatricians can diagnose and manage GERD with medication or dietary adjustments.
- Rapid Letdown: For some breastfeeding mothers, a forceful letdown reflex can overwhelm a newborn, causing them to gulp air and become fussy. Adjusting feeding positions and offering frequent burping breaks can help manage rapid letdown.
- Building Confidence: A Collaborative Approach
- While the information provided can equip mothers to identify signs of overfeeding, addressing these concerns can be emotionally charged. Here are some additional points to foster confidence and a sense of control:
- Individualized Growth Patterns: It’s important to remember that babies grow at different rates. Pediatricians track growth on percentile charts, providing valuable context for weight gain. A rapid gain for one baby might be perfectly normal for another.
- Focus on Cues, Not Volume: Rather than fixating on ounces or minutes spent feeding, the focus should be on the baby’s cues. Are they feeding actively and then showing signs of satiety? This approach reduces anxiety and promotes a more relaxed feeding experience.
- Embrace Cluster Feeding: Newborns, especially breastfed babies, may go through periods of frequent feeding, known as cluster feeding. This is a normal developmental phase that helps establish milk supply. While it can feel overwhelming, it’s a temporary phase and doesn’t necessarily indicate overfeeding.
- Support Systems Matter: New motherhood can be isolating. Don’t hesitate to seek support from partners, family members, or lactation consultants. Sharing experiences and concerns can alleviate anxieties and provide valuable insights.
Remember, you are not alone!
Most mothers experience some degree of worry regarding infant feeding. By understanding the signs of overfeeding, implementing responsive feeding practices, and collaborating with healthcare professionals, mothers can build confidence in their ability to nourish their babies and nurture healthy eating habits from the very beginning.